For years, we’ve been taught to measure health with external metrics: the number on the scale, our BMI, or the size of our jeans. While these can offer some insight, they don’t tell the whole story. True health is determined by what’s happening inside your body—how your cells are functioning, how your body produces and uses energy.
This internal world is the realm of metabolic health.
Think of your body as an engine. Metabolic health is a measure of how efficiently that engine can convert fuel (the food you eat) into energy to power everything you do. When it’s running smoothly, you feel great: stable energy, clear thinking, and a natural ability to maintain a healthy weight.
When it’s not, the engine sputters. This can manifest as afternoon energy crashes, persistent brain fog, stubborn weight gain, and intense cravings. More importantly, poor metabolic health is a precursor to some of the most common chronic diseases, including type 2 diabetes, heart disease, stroke, and Alzheimer's disease.
Understanding your metabolic health is one of the most powerful steps you can take toward a longer, healthier life. Let's start by looking at the data from your body’s own dashboard which we can get from some standard blood test results and then we will look at how we can improve our metabolic health.
Your Metabolic Dashboard: The 5 Key Markers to Watch
A simple blood test can give you a crystal-clear picture of your engine's performance. These numbers aren’t just for your doctor to see; they are vital pieces of information for you. Here are the five key markers that define your metabolic health and what their values actually mean.
1. Fasting Glucose
This is the most basic measure of your blood sugar. It tells you how much sugar (glucose) is circulating in your blood after an 8-12 hour fast. It’s a snapshot of how well your body manages its immediate fuel supply.
- What it means: High fasting glucose suggests your body isn't effectively clearing sugar from your blood, which is a classic sign that something is metabolically off.
- Optimal: <90 mg/dL
- Standard Normal: <100 mg/dL
- Pre-diabetes: 100−125 mg/dL
- Diabetes: ≥126 mg/dL
2. Fasting Insulin
If glucose is the fuel, insulin is the key that unlocks your cells to let the fuel in. Your pancreas releases insulin in response to rising blood sugar. A fasting insulin test measures how much insulin is in your blood when you haven't eaten.
- What it means: High fasting insulin is a major red flag. It means your pancreas is working overtime to produce tons of insulin because your cells are starting to ignore its signal. This is the definition of insulin resistance and it often appears years before blood sugar levels begin to rise.
- Optimal: <5 µIU/mL
- Some Insulin Resistance: 10−15 µIU/mL
- Significant Insulin Resistance: >15 µIU/mL
- Note: The "standard" range can go as high as 25 µIU/mL, which is far from optimal
3. HOMA-IR (Homeostatic Model Assessment of Insulin Resistance)
This isn't a direct measurement, but a calculation using your fasting glucose and fasting insulin levels. It provides one of the most accurate assessments of your level of insulin resistance and how hard your body is working to manage your blood sugar.
- What it means: This score gives you a more complete picture than either glucose or insulin alone. It directly quantifies your degree of insulin resistance.
- How it's calculated: (Fasting Insulin in μIU/mL×Fasting Glucose in mg/dL)/405
- Optimal (Excellent Insulin Sensitivity): <1.0
- Early Insulin Resistance: >1.9
- Significant Insulin Resistance: >2.9
4. Hemoglobin A1c (HbA1c)
Think of this as your 3-month blood sugar average. As glucose travels through your blood, it naturally sticks to your red blood cells (this process is called glycation). The HbA1c test measures the percentage of your red blood cells that have become sugar-coated. Since red blood cells live for about three months, this gives you a long-term view, smoothing out daily fluctuations.
- What it means: This is the gold-standard marker for diagnosing pre-diabetes and diabetes because it shows your average blood sugar control over a longer period.
- Optimal: <5.4%
- Standard Normal: <5.7%
- Pre-diabetes: 5.7%−6.4%
- Diabetes: ≥6.5%
5. Triglyceride / HDL Ratio
This simple ratio is an incredibly powerful predictor of both insulin resistance and your risk for heart disease. Triglycerides are fats circulating in your blood for energy, while HDL is the "good" cholesterol that cleans up excess cholesterol.
- What it means: When you're insulin resistant, your liver tends to pump out more triglycerides, and your HDL levels often drop. A high ratio is therefore a strong sign that your body isn't processing energy efficiently.
- How it's calculated: Triglycerides (in mg/dL)/HDL (in mg/dL)
- Optimal: <1.0
- Good: <2.0
- High Risk: >3.0
- Very High Risk: >5.0
You Are in the Driver's Seat
These numbers are not your destiny but give a snapshot on your metabolic health when the blood test is taken. They provide a roadmap, showing you exactly where you are currently and can be used to point you in the direction to improve your health.
Now let's look at how to improve these markers and chase optimal metabolic health.
Your Action Plan for A+ Metabolic Health
Improving your metabolic health isn't about a fad diet or a 30-day challenge. It's about implementing sustainable strategies that directly target the root cause of metabolic dysfunction: poor glucose control and chronic hyperinsulinemia (too much insulin).
Every tactic that follows is designed to do one thing: help your body manage energy more efficiently, keeping your blood sugar stable and giving your pancreas a much-needed break. Let's build your action plan.
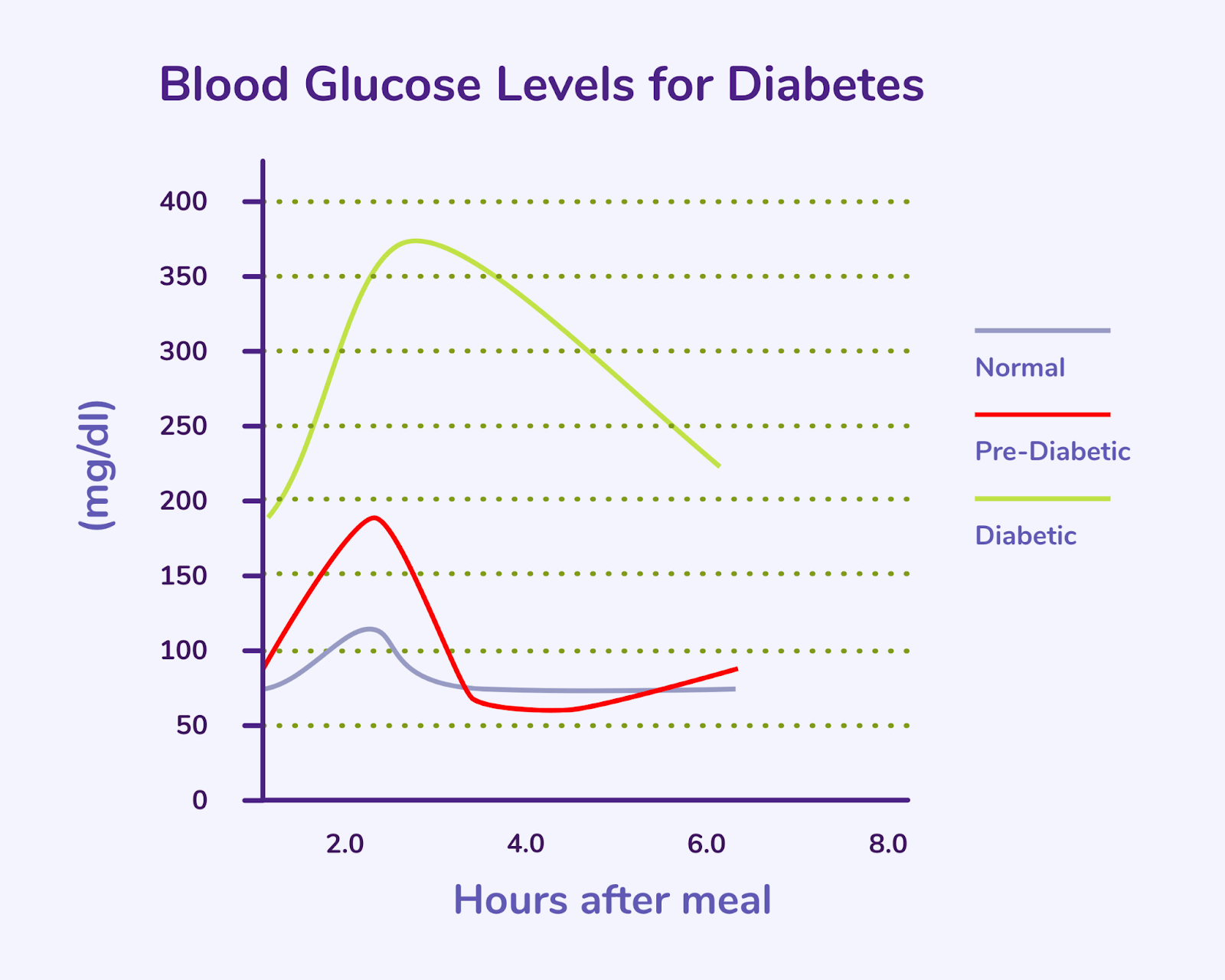
The Foundational Goal: Flatten Your Glucose Curves
Imagine your blood sugar after a meal as a wave. For a metabolically unhealthy person, eating processed carbs creates a massive tidal wave—a sharp spike followed by a dramatic crash. This sends your insulin into overdrive and leaves you feeling tired and hungry.
A metabolically healthy person's wave is just a gentle ripple. Their body handles the glucose load efficiently without a huge insulin surge. Your goal is to turn your tidal waves into ripples. Here’s how.
Pillar 1: Exercise, The Metabolic Multi-Tool
Exercise is the most potent tool you have. It works immediately and has long-term benefits by fundamentally changing how your body uses energy. The optimal strategy combines two distinct types of training.
Strength Training: Build a Bigger Glucose Sink
Think of your muscles as sponges for glucose. When you eat carbs, the resulting glucose in your blood needs to go somewhere. Your muscles are the primary storage destination. The more muscle mass you have, the bigger your "glucose sink."
- How it works: Lifting heavy weights does two things. First, it makes your muscles more sensitive to insulin, so they can absorb glucose more effectively. Second, it builds more muscle tissue, literally creating more storage space for glucose to be tucked away instead of wreaking havoc in your bloodstream.
- The Research: Countless studies, like this one from the Journal of Applied Physiology, have shown that resistance training significantly improves insulin sensitivity, often in a matter of weeks.
- Your Action Plan: Aim for 2-4 strength training sessions per week. Focus on compound movements that use multiple muscle groups (squats, deadlifts, push-ups, rows) to get the most metabolic bang for your buck.
Cardio (Zone 2): Upgrade Your Cellular Engines
While strength training builds the storage tanks, steady-state cardio upgrades the engines inside your cells: the mitochondria.
- How it works: Zone 2 cardio is a low-intensity pace where you can comfortably hold a conversation and trains your mitochondria to become incredibly efficient at burning fat for fuel. This "metabolic flexibility" means your body doesn't have to rely solely on glucose for energy. Better fat oxidation means less demand on your glucose-management system throughout the day.
- The Research: Research shows that this type of endurance exercise increases both the number and efficiency of mitochondria, fundamentally improving your body's ability to use fuel.
- Your Action Plan: Aim for 3-4 sessions of 45-60 minutes of Zone 2 cardio per week. This could be a brisk walk on an incline, a light jog, cycling, or using an elliptical.
Pillar 2: Nutrition, Fueling for Stability
You can't out-train a bad diet. Your nutritional strategy should focus on minimizing glucose spikes and reducing the overall burden on insulin.
Meal Sequencing: Eat Your Veggies First
This is the simplest and most effective nutritional hack you can implement. The order in which you eat your macronutrients has a profound impact on your blood sugar response.
- How it works: Starting your meal with fiber (vegetables), fat (olive oil, avocado), and protein creates a kind of "buffer" in your stomach. As shown in groundbreaking research from Dr. Alpana Shukla, this slows down gastric emptying and the absorption of carbohydrates, leading to a much smaller, gentler glucose curve.
- Your Action Plan: Before you touch the pasta, bread, or rice, eat your salad, non-starchy vegetables, and protein source first. Save your starches and sugars for the end of the meal.
Carb Management, Not Elimination
You don't necessarily have to "avoid" carbs, but you must be strategic. The type of carbohydrate matters immensely.
- How it works: A sugary soda is a glucose bomb. A bowl of lentils is not. The difference is fiber. Fiber-rich, whole-food carbohydrates are broken down slowly, leading to a minimal blood sugar response. Ultra-processed carbs are digested almost instantly, sending your blood sugar soaring.
- Your Action Plan: Swap processed carbs for whole-food versions. Ditch the white bread for stone-ground whole wheat, the sugary cereal for oatmeal, and the fruit juice for whole fruit.
Time-Restricted Eating (TRE): Give Your System a Break
TRE isn't about what you eat, but when you eat. By compressing your daily eating into an 8-10 hour window, you give your body a longer period of fasting.
- How it works: Every time you eat, you trigger an insulin response. By giving your body a 14-16 hour break from food, your insulin levels can drop to a low baseline and stay there. This extended break is critical for resensitizing your cells to insulin's signal, directly combating insulin resistance.
- The Research: Studies from institutions like the Salk Institute have consistently shown that TRE can improve insulin sensitivity, reduce blood pressure, and aid in weight management, even without changing what people eat.
- Your Action Plan: Start by simply aiming for a 12-hour fast overnight (e.g., 8 PM to 8 AM). Once that's comfortable, gradually try to extend the fasting window by pushing your first meal later or eating your last meal earlier.
Pillar 3: Lifestyle, The Non-Negotiable Foundation
Exercise and nutrition are crucial, but they can be undermined if your underlying lifestyle is working against you. These factors are foundational to your metabolic health.
Post-Meal Movement: The 10-Minute Glucose Hack
One of the most powerful ways to blunt a glucose spike is to use your muscles right after you eat.
- How it works: When you contract your muscles they can pull glucose directly from your bloodstream for energy without needing insulin. This acts as a biological "hack" to immediately lower your post-meal blood sugar.
- Your Action Plan: Aim for a 10-20 minute gentle walk within an hour of finishing your meals, especially those higher in carbohydrates. Even doing bodyweight squats or calf raises at your desk can make a meaningful difference.
Sleep: Your Nightly Metabolic Reset 😴
Sleep isn't a luxury; it's a critical metabolic process. Poor sleep is one of the fastest ways to destroy your insulin sensitivity.
- How it works: Sleep deprivation raises the stress hormone cortisol, which tells your body to release more glucose. Research has shown that even a single night of poor sleep can induce a state of insulin resistance comparable to that of a pre-diabetic individual. It also dysregulates your hunger hormones, making you crave high-sugar, high-fat foods.
- Your Action Plan: Prioritize 7-9 hours of high-quality sleep. Create a non-negotiable sleep routine: keep your room dark, cool, and quiet, and try to go to bed and wake up at the same time every day.
Stress Management: Taming the Cortisol Response
Your body can't tell the difference between being chased by a predator and being stressed about a work deadline. The physiological response is the same: a flood of cortisol.
- How it works: Chronic stress leads to chronically elevated cortisol. Cortisol's primary job is to ensure you have enough energy (glucose) available to handle a threat. It tells your liver to dump sugar into the bloodstream. If you're not physically fighting or fleeing, that sugar has nowhere to go, leading to high blood sugar and a constant demand for insulin.
- Your Action Plan: Incorporate a daily stress-management practice. This could be meditation, breathwork (like the physiological sigh), spending time in nature, or journaling. The goal is to activate your parasympathetic "rest-and-digest" nervous system to counteract the "fight-or-flight" response.
The Takeaway: Consistency Trumps Perfection
You have the data. You have the tools. The key now is implementation. Don't try to do everything at once. Pick one or two strategies, like adding a 20-minute walk after dinner and eating your salad first, and master them.
These interventions are powerful because they work together, creating a positive feedback loop that builds a resilient, efficient, and healthy metabolic engine.
-Jake