There is a distinct paradox in modern health. We currently have access to more calories and food options than any civilization in history, yet from a biochemical standpoint, we are starving.
Data from the National Health and Nutrition Examination Survey consistently paints a concerning picture. Despite high caloric intake, a vast majority of Americans are failing to meet the Recommended Daily Allowance for essential micronutrients. This isn't just about eating "junk food." It is a systemic issue involving soil depletion, modern food processing, and a lifestyle that demands high nutrient output while providing low nutrient input.
We are effectively running high-performance machinery on diluted fuel. When you lack these foundational raw materials, your body doesn't necessarily shut down immediately. Instead, it downregulates. It prioritizes immediate survival over long-term repair, mood regulation, and energy production.
Here are the four most common nutritional gaps likely widening in your body right now, and the science-backed ways to close them.
1. Magnesium: The Master Regulator
Magnesium is not just a mineral to help you sleep. It is an essential cofactor in over 300 enzymatic reactions. It is the ignition key for ATP production (energy), acts as the primary regulator of electrolyte balance, and physically governs the relaxation of muscle tissue and blood vessels.
The Science:
Current estimates suggest nearly half of the US population consumes less than the required amount of magnesium [1]. This is largely due to modern agricultural practices. As we have bred crops for yield and size, and as soil quality degrades, the magnesium content in vegetables has dropped significantly over the last 50 years. Simultaneously, metabolic stressors like high sugar intake and chronic stress deplete the magnesium you do have, increasing urinary excretion of the mineral.
Testing:
- The Test: Standard serum magnesium tests are notoriously inaccurate because the body tightly regulates magnesium levels in the blood, often pulling it from bone stores to keep serum levels "normal." A more sensitive, though less commonly ordered, test that we recommend is Red Blood Cell Magnesium (Magnesium RBC).
Check out GoodLabs for all your blood testing needs while also supporting a company trying to democratize blood testing for everyone - Standard "Normal" Range: Serum levels are usually 1.7–2.2 mg/dL and Magnesium RDW normal range is 4-6.4 mg/dL
- Longevity Optimal Range: Magnesium RBC levels should be in the upper half of the reference range targeting >5 mg/dL [2]
The Fix:
- Food First: Focus on chlorophyll-rich foods. If it is dark green and leafy (spinach, chard), it is likely high in magnesium. Pumpkin seeds and almonds are also dense sources.
- Supplementation: Because it is difficult to reach therapeutic levels through food alone, supplementation is often necessary. Avoid Magnesium Oxide, which has poor bioavailability. Opt for Magnesium Glycinate for general relaxation and absorption, Magnesium Taurate to get some taurine, or Magnesium L-Threonate, which is the only form shown to effectively cross the blood-brain barrier to support cognitive function.

2. Omega-3 Fatty Acids: The Membrane Builder
For years the conversation on fat was about quantity. We now know the quality and source matter far more. Your cell membranes are made of fat. The lipid bilayer that protects your cells and allows for cellular communication depends on a specific balance of fatty acids to remain fluid and permeable.
The Science:
Anthropological data suggests humans evolved with an Omega-6 to Omega-3 ratio of roughly 1:1. Omega-6s (pro-inflammatory) trigger necessary immune responses, while Omega-3s (anti-inflammatory) resolve them. Today, due to the ubiquity of industrial seed oils like soybean and corn oil, the average American ratio is closer to 20:1. This creates a state of chronic, low-grade inflammation because the body lacks the EPA and DHA required to resolve the inflammatory response [3].
Testing:
- The Test: The Omega-3 Index via OmegaCheck is the definitive test. It measures the percentage of EPA and DHA in your red blood cell membranes, giving a reliable, long-term measure of your intake.
With GoodLabs order the OmegaCheck test which includes: EPA + DPA + DHA, Arachidonic Acid/EPA Ratio, Omega-6/Omega-3 Ratio, Omega-3 Total, EPA, DPA, DHA, Omega-6 Total, Arachidonic Acid, and Linoleic Acid - Standard "Normal" Range: > 4%.
- Longevity Optimal Range: > 8%. (Risk is highest below 4%, and benefit is maximized above 8%.) [4]
The Fix:
- Food First: Aggressively reduce intake of seed oils (found in most processed foods and salad dressings). Replace them with olive oil, avocado oil, or butter. Increase consumption of cold-water fatty fish like salmon, mackerel, or sardines.
- Supplement as needed: Let’s be honest not everyone is going to get enough Omega 3’s through diet and will need to supplement to hit ideal values. I like Viva Naturals, Nordic Naturals, and Carlson
- The Metric: Aim for an Omega-3 Index of >8%. Most Americans sit near 4%, placing them at significantly higher risk for cardiovascular events [4]

3. Vitamin D: The Genetic Key
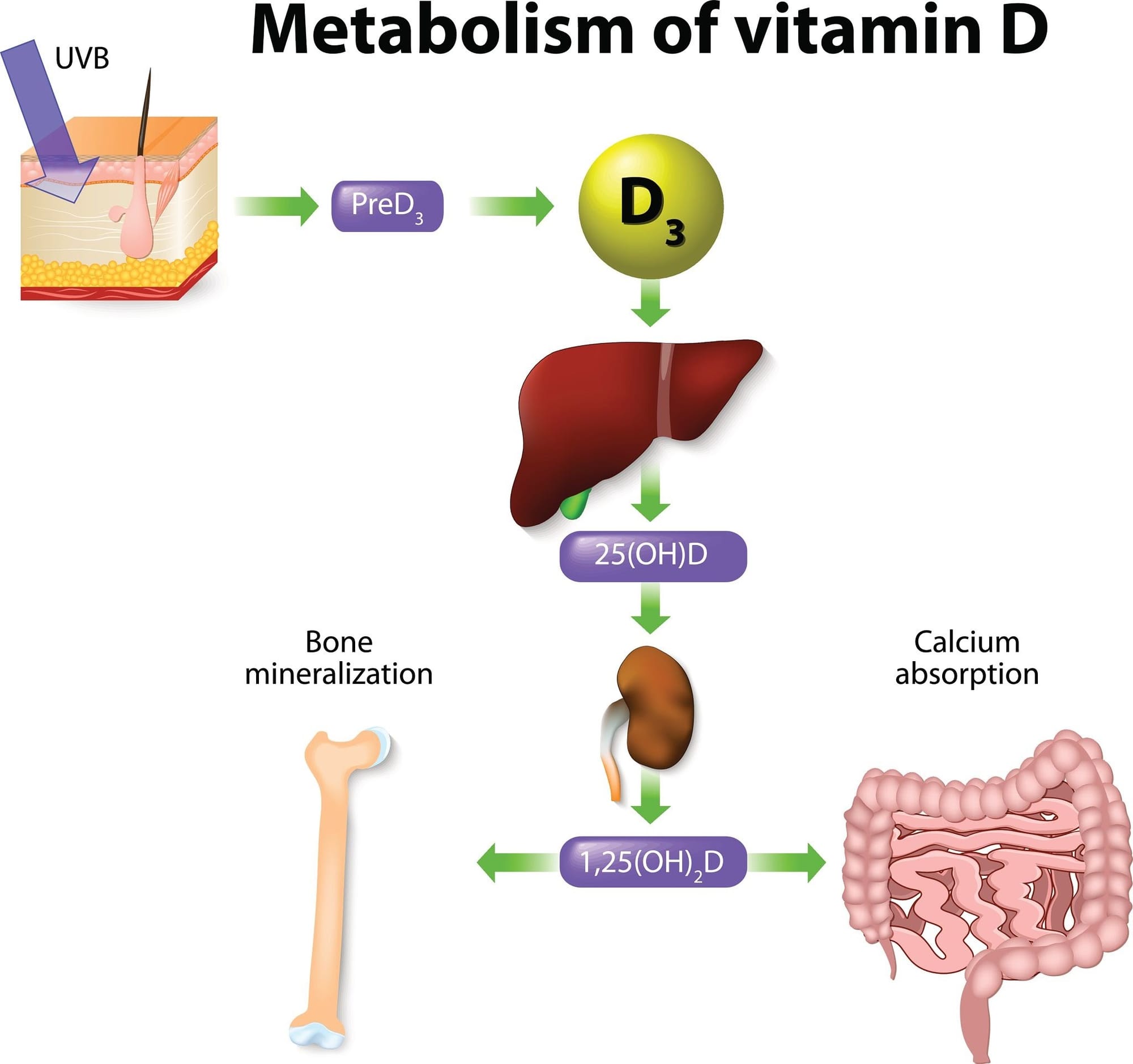
Referring to Vitamin D as a vitamin is technically a misnomer. It is a pro-hormone synthesized in the skin via UV exposure. Once converted to its active form, it travels to the nucleus of your cells and regulates the expression of over 1,000 genes, influencing everything from immune defense to bone density and mood regulation.
The Science:
Our shift to an indoor existence has decimated our Vitamin D levels. NHANES data indicates that roughly 40% of US adults are clinically deficient, with even higher rates in darker-skinned populations (as melanin reduces UV absorption) [5]. Suboptimal levels are linked to increased all-cause mortality, higher susceptibility to respiratory infections, and mood disorders.
Testing:
- The Test: 25-Hydroxyvitamin D (25(OH)D) is the standard and correct test to measure your body's circulating storage levels. As with all other tests I like GoodLabs
- Standard "Normal" Range: Typically defined as > 30 ng/mL.
- Longevity Optimal Range: 40–60 ng/mL. The lowest all-cause mortality risk is consistently found in this range [6]
The Fix:
- Sunlight: While ideal, consistent midday sun exposure is difficult for many due to latitude and work schedules.
- Supplementation: This is one of the few nutrients where supplementation is almost mandatory for those living away from the equator. Pairing Vitamin D3 with K2 is critical. K2 ensures that the calcium mobilized by Vitamin D is deposited in your bones rather than calcifying your arteries. I like Pure and Sports Research as they combine the D3 and K2 into a single pill.
4. Potassium: The Sodium Antagonist
We hear constantly about the dangers of sodium, but sodium is only half the story. In the body, sodium and potassium operate on a seesaw. The issue isn't just that we eat too much salt; it is that we eat dangerously little potassium. This imbalance drives high blood pressure and vascular stiffness.
The Science:
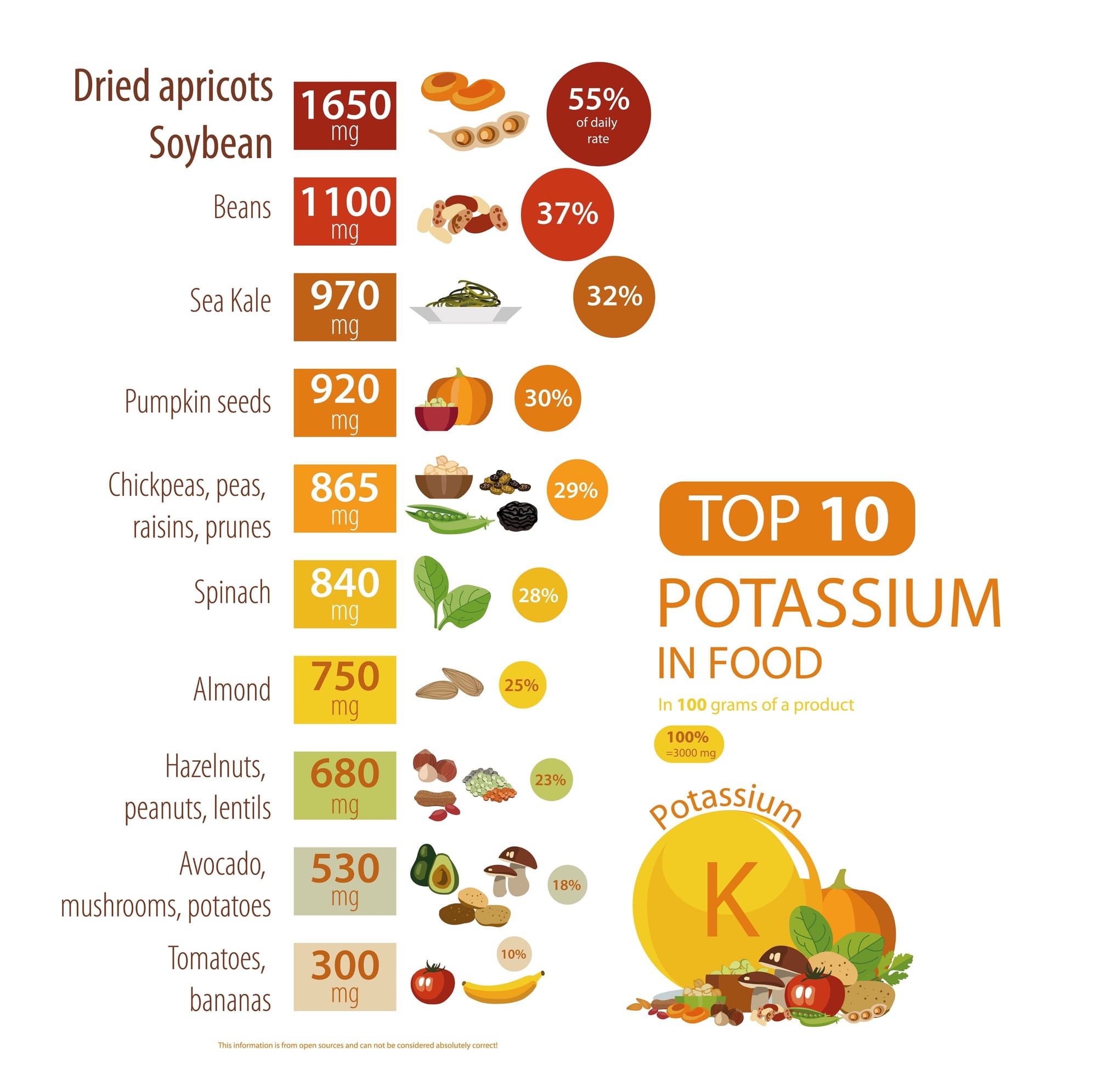
Our ancestors likely consumed over 10,000 mg of potassium a day from a diet heavy in roots, tubers, and fruits. Today, less than 3% of Americans meet the mere 4,700 mg recommendation [7]. This creates a "cation imbalance" that forces the body to retain fluid and increases pressure on the kidneys and arterial walls. This imbalance is a primary, but often unrecognized, driver of hypertension.
Testing:
- The Test: Serum Potassium (part of a standard electrolyte panel) is useful, but like magnesium, it is tightly regulated. A better proxy for long-term status is the Sodium-to-Potassium Ratio derived from a 24-hour urine collection or a spot urine test.
- Standard "Normal" Range: Serum levels are usually 3.5–5.0 mEq/L.
- Longevity Optimal Range: A 24-hour urine Sodium-to-Potassium Ratio of less than 2.0.
The Fix:
- Food First: You cannot supplement your way out of a potassium deficiency easily, as laws restrict supplement potency to extremely low doses (usually 99mg) for safety reasons. You must eat it. Prioritize avocados, sweet potatoes, white beans, spinach, and salmon.
- The Strategy: Rather than just cutting salt, focus on doubling your intake of potassium-rich plant foods. This naturally rebalances the sodium-potassium ratio and lowers blood pressure more effectively than sodium restriction alone.
The Takeaway
The solution to these deficiencies isn't a handful of pills to mask a poor diet. Supplements are tools to bridge the gap, not pave the road. The goal is to construct a diet that prioritizes nutrient density over caloric density, ensuring your body has the raw materials it requires to function at its peak. Start by addressing these four critical gaps.
Sources:
[1] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5897105/
[2] https://www.mdpi.com/2072-6643/10/12/1863
[3] https://pubmed.ncbi.nlm.nih.gov/12442909/
[4]https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.116.024314
[5] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6075634/
[6] https://www.nejm.org/doi/full/10.1056/NEJMe078047
[7] https://academic.oup.com/ajcn/article/81/2/341/4649721
[8] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6647167/

